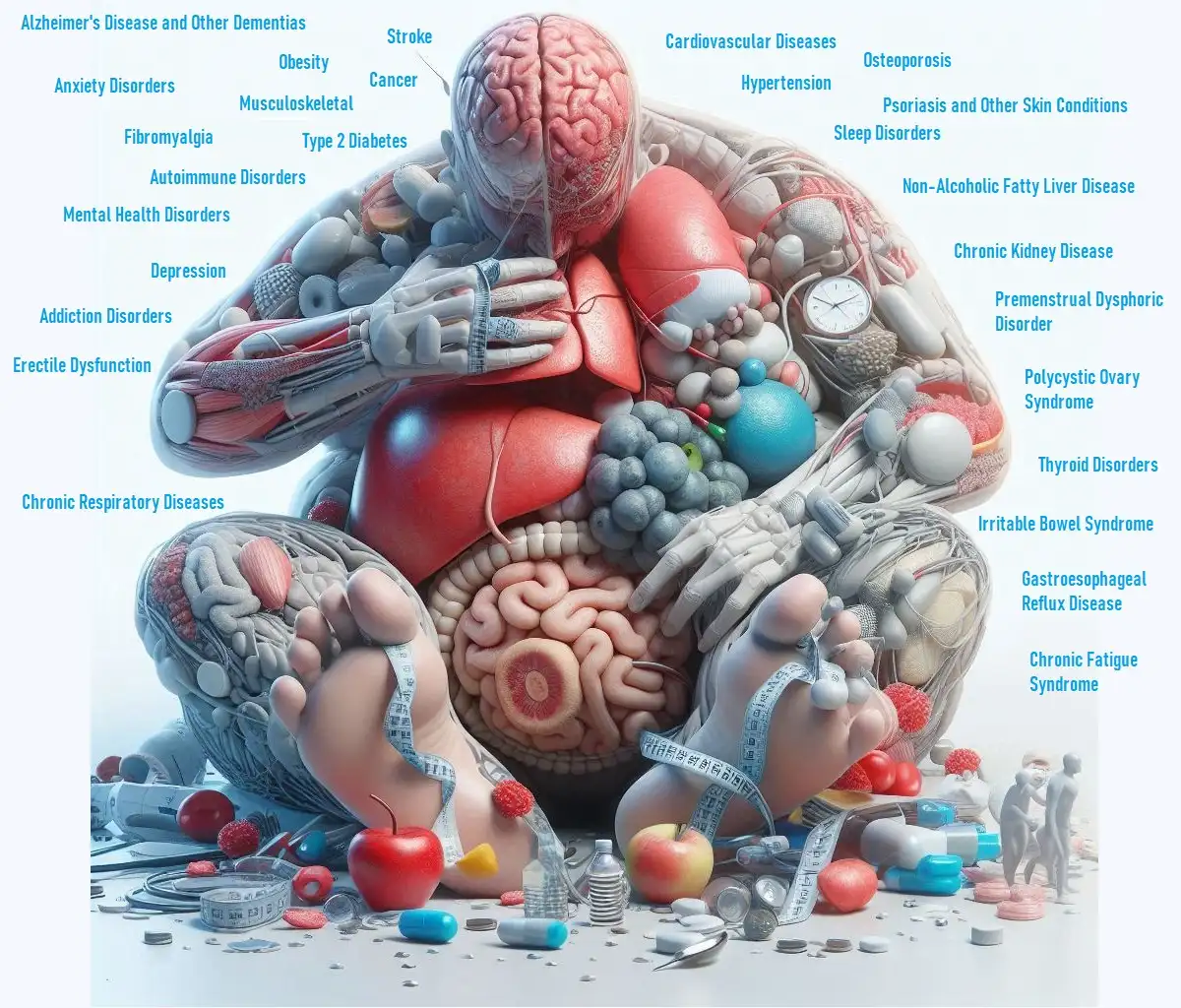
Understanding how to maintain good gastrointestinal health can be complex, but it’s crucial for overall well-being. Digestive issues such as Irritable Bowel Syndrome (IBS), acid reflux, and Small Intestinal Bacterial Overgrowth (SIBO) can significantly impact your quality of life. This guide explores the roles of gut microbiota, diet, inflammation, and digestive enzymes in managing these conditions effectively.
Key Takeaways
- Gut microbiota influences your digestive health and can impact conditions like IBS and SIBO.
- The FODMAP diet can help manage IBS symptoms by avoiding certain types of fermentable carbohydrates.
- Chronic inflammation can harm your gastrointestinal system and worsen digestive disorders.
- Digestive enzymes can alleviate acid reflux symptoms by improving digestion.
- SIBO can disrupt normal digestion and lead to a range of gastrointestinal issues.
Impact of Gut Microbiota on Gastrointestinal Health
What is Gut Microbiota?
Gut microbiota refers to the diverse community of microorganisms living in your digestive tract. These bacteria, fungi, and other microbes play a crucial role in your overall health, including:
- Digestive Function: They help break down food, making nutrients more available for absorption.
- Immune System Support: A healthy microbiota supports your immune system and protects against harmful pathogens.
- Metabolism Regulation: They assist in regulating your metabolism and can influence body weight and energy levels.
How Gut Microbiota Affects Digestive Health
- Balanced Microbiota: A diverse and balanced microbiota contributes to a healthy digestive system, preventing issues like IBS and SIBO.
- Dysbiosis: An imbalance in gut bacteria, known as dysbiosis, can lead to digestive problems, including bloating, gas, and irregular bowel movements.
- Inflammation: Imbalanced gut flora can trigger inflammation, which may exacerbate conditions such as Crohn’s disease and ulcerative colitis.
Improving Gut Microbiota
- Eat a Variety of Foods: Consuming a range of fruits, vegetables, and whole grains helps promote a diverse microbiota.
- Include Probiotics: Probiotic-rich foods like yogurt, kefir, and fermented vegetables support healthy gut bacteria.
- Limit Processed Foods: Reduce intake of processed and high-sugar foods that can negatively impact gut health.
Role of FODMAP Diet in IBS Management
What is the FODMAP Diet?
The FODMAP diet focuses on reducing the intake of specific types of carbohydrates that are poorly absorbed in the small intestine. FODMAP stands for:
- Fermentable
- Oligosaccharides
- Disaccharides
- Monosaccharides
- Polyols
How the FODMAP Diet Helps IBS
- Reduces Symptoms: The FODMAP diet can help alleviate symptoms such as bloating, gas, and abdominal pain by minimizing the intake of fermentable carbohydrates.
- Identifies Triggers: It helps identify which specific foods trigger your IBS symptoms, allowing for better management.
- Improves Quality of Life: Many people with IBS find significant relief from symptoms and improved quality of life by following this diet.
Implementing the FODMAP Diet
- Follow a Structured Plan: Start with a strict elimination phase, then gradually reintroduce foods to identify triggers.
- Consult a Dietitian: Work with a registered dietitian to ensure you’re following the diet correctly and meeting your nutritional needs.
- Monitor Symptoms: Keep a food diary to track symptoms and adjust your diet as needed.
Impact of Chronic Inflammation on Gastrointestinal Health
What is Chronic Inflammation?
Chronic inflammation is a prolonged inflammatory response that can harm tissues and organs over time. In the context of gastrointestinal health:
- Damage to Gut Lining: Persistent inflammation can damage the lining of the digestive tract, leading to conditions like inflammatory bowel disease (IBD).
- Disrupted Digestion: Inflammation can disrupt normal digestion, contributing to symptoms like pain, diarrhea, and constipation.
- Immune System Effects: Chronic inflammation can impair the immune system, making you more susceptible to infections and other diseases.
Managing Chronic Inflammation
- Anti-Inflammatory Diet: Incorporate foods with anti-inflammatory properties, such as berries, leafy greens, and fatty fish.
- Avoid Triggers: Limit or avoid foods that may promote inflammation, such as processed meats, sugary snacks, and trans fats.
- Stay Active: Regular exercise has been shown to reduce inflammation and support overall health.
Role of Digestive Enzymes in Managing Acid Reflux
What are Digestive Enzymes?
Digestive enzymes are proteins that help break down food into smaller molecules, making it easier for your body to absorb nutrients. They play a key role in managing acid reflux by:
- Improving Digestion: By aiding in the breakdown of food, digestive enzymes can reduce the burden on your stomach and esophagus, which may alleviate acid reflux symptoms.
- Reducing Acid Production: Efficient digestion can help prevent excessive stomach acid production, which is a common cause of acid reflux.
Using Digestive Enzymes
- Incorporate Enzyme-Rich Foods: Foods like pineapple and papaya contain natural digestive enzymes that can aid digestion.
- Consider Supplements: Digestive enzyme supplements can be helpful if you have difficulty digesting certain foods. Consult your healthcare provider for appropriate options.
- Eat Smaller, More Frequent Meals: Eating smaller meals more frequently can help reduce acid reflux symptoms by preventing excessive stomach acid production.
Impact of SIBO on Gastrointestinal Health
What is SIBO?
Small Intestinal Bacterial Overgrowth (SIBO) occurs when there is an abnormal increase in bacteria in the small intestine. This condition can lead to a range of digestive issues, including:
- Bloating and Gas: Excess bacteria ferment undigested food, leading to bloating and gas.
- Diarrhea or Constipation: SIBO can cause changes in bowel habits, leading to diarrhea or constipation.
- Nutritional Deficiencies: The overgrowth of bacteria can interfere with nutrient absorption, leading to deficiencies.
Managing SIBO
- Follow a SIBO Diet: A low-FODMAP diet or specific carbohydrate diet can help reduce symptoms by limiting foods that fuel bacterial overgrowth.
- Use Antibiotics: Your doctor may prescribe antibiotics to reduce the bacterial overgrowth in the small intestine.
- Consider Probiotics: Probiotics may help restore a healthy balance of gut bacteria, but consult your healthcare provider for the best approach.
Conclusion
Maintaining good gastrointestinal health involves understanding the roles of gut microbiota, dietary choices, chronic inflammation, digestive enzymes, and conditions like SIBO. By addressing these factors, you can manage symptoms more effectively and improve your overall digestive well-being. Whether it’s through dietary changes, lifestyle adjustments, or medical treatments, taking a proactive approach can lead to significant improvements in your quality of life.