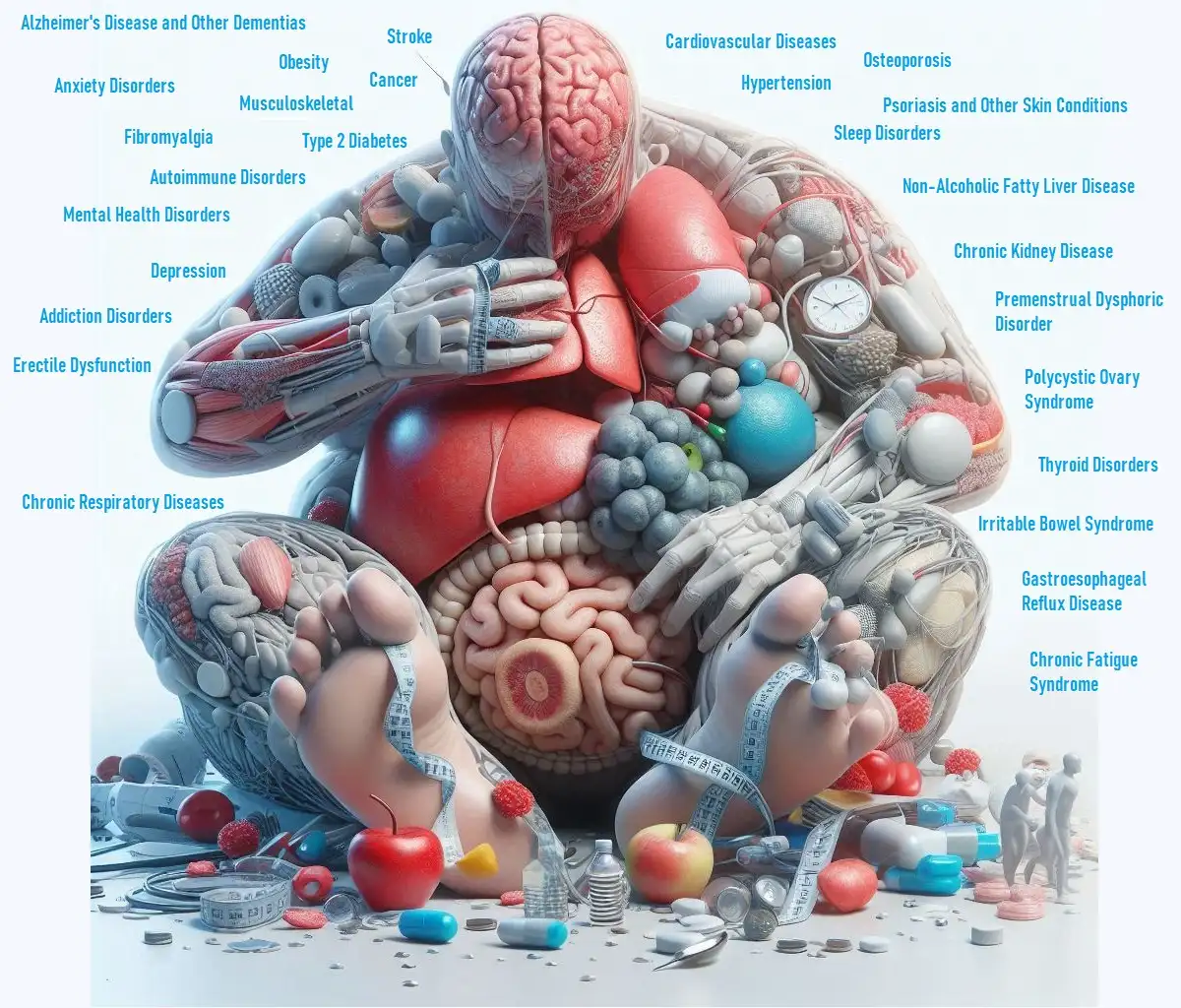
Cardiovascular health is crucial for overall well-being, but many factors can influence it beyond diet and exercise. Chronic stress, mitochondrial dysfunction, low-grade inflammation, and sleep deprivation are significant contributors to cardiovascular risk. This article explores how these factors affect heart health and what you can do to mitigate their impact.
Key Takeaways
- Chronic Stress: Can significantly harm cardiovascular function, increasing your risk of heart disease.
- Mitochondrial Dysfunction: Impairs energy production and can lead to cardiovascular problems.
- L-Carnitine: Aids in heart disease prevention by supporting energy metabolism.
- Low-Grade Inflammation: A persistent issue that negatively affects cardiovascular health.
- Sleep Deprivation: Increases cardiovascular risks and impacts overall heart health.
Impact of Chronic Stress on Cardiovascular Function
What Is Chronic Stress?
Chronic stress refers to ongoing, prolonged stress that exceeds the body’s ability to cope. Unlike acute stress, which can be short-lived, chronic stress can have long-term effects on your health, especially your heart.
- Heart Disease Risk: Chronic stress contributes to the development of heart disease by increasing blood pressure and causing inflammation. Over time, this can damage blood vessels and increase the risk of heart attacks.
- Hormonal Imbalance: Stress hormones like cortisol can disrupt normal heart function and contribute to arrhythmias (irregular heartbeats).
Managing Chronic Stress
- Stress-Reduction Techniques: Practice relaxation techniques such as deep breathing, meditation, and yoga to manage stress levels.
- Healthy Lifestyle: Regular exercise, a balanced diet, and sufficient sleep can help lower stress and improve heart health.
- Seek Support: If stress becomes overwhelming, consider talking to a mental health professional for additional support and coping strategies.
Cardiovascular Health and Mitochondrial Dysfunction
What Is Mitochondrial Dysfunction?
Mitochondria are the powerhouses of our cells, providing the energy needed for cellular functions. When mitochondria are not functioning properly, it can lead to various health issues, including cardiovascular problems.
- Energy Production: Dysfunctional mitochondria lead to decreased energy production, which can affect heart muscle function and increase the risk of heart disease.
- Oxidative Stress: Mitochondrial dysfunction can cause oxidative stress, damaging blood vessels and contributing to cardiovascular disease.
Improving Mitochondrial Function
- Healthy Diet: Consuming foods rich in antioxidants, such as fruits and vegetables, can help reduce oxidative stress.
- Exercise: Regular physical activity supports mitochondrial health and enhances energy production.
- Supplements: Certain supplements, like CoQ10, may support mitochondrial function and cardiovascular health. Consult with a healthcare provider before starting any new supplements.
Role of L-Carnitine in Heart Disease Prevention
What Is L-Carnitine?
L-carnitine is an amino acid that plays a key role in energy metabolism by transporting fatty acids into the mitochondria, where they are converted into energy. It has been studied for its potential benefits in heart disease prevention.
- Energy Metabolism: L-carnitine helps improve energy production in heart cells, potentially reducing the risk of heart disease.
- Heart Health: Research suggests that L-carnitine supplementation can improve exercise tolerance and reduce symptoms of heart disease.
How to Use L-Carnitine
- Supplement Form: L-carnitine is available in various forms, including capsules and powders. Follow dosage recommendations on the label or as advised by your healthcare provider.
- Dietary Sources: L-carnitine is found in foods like red meat and dairy products. Including these in your diet can help maintain adequate levels.
Impact of Low-Grade Inflammation on Cardiovascular Health
What Is Low-Grade Inflammation?
Low-grade inflammation is a chronic, low-level inflammation that persists over time and can be a silent contributor to cardiovascular disease.
- Cardiovascular Risk: Persistent inflammation can damage blood vessels, leading to atherosclerosis (hardening of the arteries) and increasing the risk of heart attacks and strokes.
- Inflammatory Markers: High levels of inflammatory markers, such as C-reactive protein (CRP), are associated with an increased risk of cardiovascular events.
Reducing Low-Grade Inflammation
- Anti-Inflammatory Diet: Eat foods rich in anti-inflammatory nutrients, such as omega-3 fatty acids, found in fatty fish, and antioxidants in fruits and vegetables.
- Regular Exercise: Engaging in physical activity can help reduce inflammation and improve overall cardiovascular health.
- Healthy Weight: Maintaining a healthy weight is crucial for managing inflammation and reducing cardiovascular risk.
Cardiovascular Risks of Sleep Deprivation
How Sleep Affects Cardiovascular Health
Sleep deprivation, or not getting enough restful sleep, can have a serious impact on heart health.
- Increased Risk: Chronic lack of sleep is linked to higher risks of high blood pressure, heart disease, and stroke.
- Hormonal Imbalance: Sleep deprivation can lead to hormonal imbalances that negatively affect heart health, including increased levels of stress hormones and inflammation.
Improving Sleep Quality
- Sleep Hygiene: Establish a regular sleep schedule, create a relaxing bedtime routine, and make your sleep environment comfortable.
- Limit Stimulants: Avoid caffeine and electronic screens before bed to improve sleep quality.
- Seek Help: If you have persistent sleep issues, consider consulting a healthcare provider to address any underlying conditions.
Conclusion
Understanding how chronic stress, mitochondrial dysfunction, and lifestyle factors like sleep and diet impact cardiovascular health is crucial for preventing heart disease and maintaining overall well-being. By addressing these areas—through stress management, supporting mitochondrial function, and improving sleep—you can take significant steps toward better heart health.
Remember to consult with your healthcare provider before making any significant changes to your health routine. Integrating these insights into your daily life can lead to improved cardiovascular health and a better quality of life.